A Pathogen Too Far: How the 1918 Pandemic Revolutionized Virology

In 1918, epidemic disease and war once again embraced with all their old passion. The deadly pandemic that began that year became known as the Spanish flu because Spain was a neutral country, and its press was the first to report the devastating outbreak. The warring countries meanwhile suppressed the news, leaving their citizens unprepared. This flu was particularly terrifying because it spread so easily and because it concentrated its venom on the young. (Their elders may have acquired immunity from exposure to a previous flu outbreak.) It filled up its victims’ lungs with fluid, and the desperate hunger for air turned their skin blue as they suffocated.
The first of three waves hit soldiers in France early in 1918. But the flu soon spread from there, in two subsequent and far more virulent waves, to sicken soldiers and civilians almost everywhere. Over the course of two years, it infected an estimated 500 million people worldwide, a quarter to a third of the human population, and killed 50 million of them, with most of the dead between 20 and 40 years of age. (By comparison, the COVID-19 pandemic has infected about 750 million people at this writing — under 10 percent of the current human population.)
In most fatal cases, the immediate cause of death was pneumonia, marked by an abundance of Streptococcus, Staphylococcus, and other bacteria. But something else seemed to be preparing the way for these common microbes to proliferate. As a later physician put it, “The specific virus ploughs the land and the secondary bacteria germinate in the furrows.”
As one physician put it, “The specific virus ploughs the land and the secondary bacteria germinate in the furrows.”
A half century of germ theory and triumphant bacteriology led almost everyone to suspect a bacterial, not a viral, pathogen. In fact, they suspected one specific bacterial pathogen. Haemophilus influenzae was also known as Pfeiffer’s bacillus, for Richard Pfeiffer, a researcher at the Robert Koch Institute, who had identified it as the cause of an 1889–1890 influenza pandemic. Pfeiffer’s indictment of this bacillus went largely unquestioned for a quarter century, until the bodies started to pile up in 1918. Researchers around the world then searched desperately for H. influenzae in victims of the new pandemic, with little success. Pfeiffer himself admitted that he could find it in only about half of flu victims. Other scientists found it but couldn’t get it to produce flu even when sprayed as a pure culture into the respiratory tracts of monkeys and human test subjects.
Going Viral
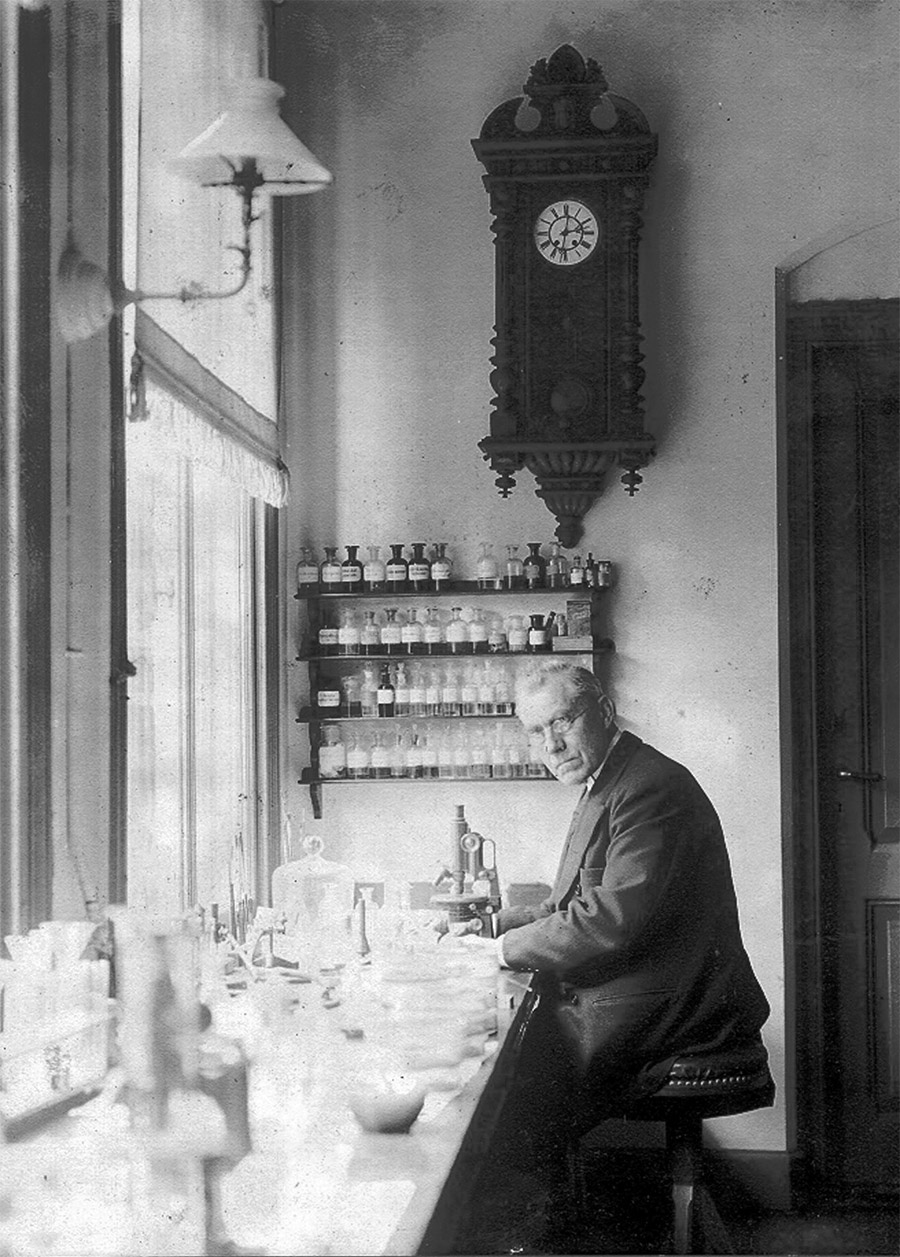
The failure of Pfeiffer’s bacillus — the failure of bacteriology — led some researchers to think back 20 years to a different and still relatively obscure line of microbial research. In 1898, Martinus Beijerinck (1851–1931), a microbiologist in Delft, The Netherlands, was studying a disease of tobacco plants. Beijerinck took an extract from plants infected with tobacco mosaic and put it through a Chamberland filter to screen out bacteria and other contaminants. With the filtered extract, he infected other plants, then took filtered extracts from those plants and infected still other plants, and so on in a series. Beijerinck thought the contagium consisted of nothing more than dissolved molecules. So how to explain its reproductive capabilities? He concluded that it “must be incorporated into the living protoplasm of the cell, into whose reproduction it is, in a manner of speaking, passively drawn.” This must have seemed to his contemporaries like a wildly improbable speculation. In fact, though, it fits remarkably well with the modern understanding of how a virus reproduces. What may also seem wildly improbable was that Beijerinck developed this first good description of a virus within a short walk of where Antoni van Leeuwenhoek had seen and described the first known bacteria. Thus Delft secured its place, over a distance of more than 200 years, as the cradle of microbiology.
That same year, a German team led by Friedrich Loeffler, who had previously discovered the bacterial agent of diphtheria, used filtration to identify the first animal virus, for foot-and-mouth disease. And in 1901 in Cuba, Americans James Carroll (1854–1907) and Walter Reed (1851–1902) demonstrated that the agent of yellow fever remained infectious after passing through a bacteria-proof filter, making it the first known human disease caused by a virus. (This was a footnote to their previous work demonstrating that yellow fever, like malaria, was a mosquito-borne disease.) By 1906, at least 18 such pathogens affecting plants, animals, or humans were known. Contemporaries called them filter-passing, or filterable, pathogens, or increasingly just viruses. But it would be years before anybody could see one or describe one morphologically or chemically. Virology meantime remained clouded in confusion and doubt.
The 1918 pandemic pushed researchers to look more closely and think much harder about this new science. Different research groups began to apply their Chamberland filters to samples from flu victims. Charles Nicolle and Charles Lebailly at the Pasteur Institute in Tunisia were the first to report success, in October 1918, after using filtered sputum from a flu victim to pass the disease to two volunteer test subjects. In Germany, two researchers tested a filtrate from a flu victim on themselves, with unknown results; and in Flanders, a British researcher died while experimenting with a filtrate. In Japan, researchers exposed 24 volunteers — “our friends, doctors and nurses” — to the flu, some with an emulsion of fluids straight from victims of the pandemic, others with a filtered extract. Six who had recovered from the flu showed no signs of a recurrence. The other 18, who were new to the disease, all came down with flu, in some cases with “very severe” symptoms. The filtered extract was equal to the emulsion as a source of contagion.
Skepticism persisted, however, with some critics still arguing well after the war that “the invisible virus concept” was little more than a ruse to absolve “the discoverers from the necessity of producing evidence of a characteristic microbe.” When a few researchers attempted to develop a flu vaccine in 1918, they worked instead with attenuated bacteria. Older defensive measures — quarantine and closures of schools, churches, movie theaters, and restaurants — proved more effective in bringing the pandemic to a close. That, and what may be the oldest measure: By 1920, almost all potential victims had acquired immunity by surviving the flu — or dying.
The pandemic launched medical thinking in a dramatically new direction over the next decade and, indeed, for the remainder of the 20th century. Having been routed by influenza, medical researchers now regrouped to address the puzzle of filter-passing viruses. “There could hardly be a set of problems whose solution has more potential importance for the community than this,” the secretary of the British Medical Research Council declared in 1922, noting that “in a few months in 1918–1919 [flu] killed more persons in India than had died from the plague there during the previous 20 years.” It was the beginning of a major initiative to apply “new technical methods of investigation” to viruses.
By 1920, almost all potential victims had acquired immunity by surviving the flu — or dying.
Other developed nations also pursued viral research, and by 1927, a Rockefeller Institute researcher could list close to 100 diseases thought to be viral, though he allowed plenty of room for subtractions from this list, on the reasonable assumption that some would later turn out to be caused by very small bacteria or protozoa. Among those affecting humans, the list correctly included smallpox, chicken pox, herpes, encephalitis, yellow fever, dengue, polio, rabies, mumps, measles, rubella, the common cold, and influenza.
The questions about viruses that were still outstanding seem like the ones we would ask on encountering a featureless but disturbingly forceful presence from some distant planet: What does it look like? Can it mutate? Is it alive? And always the one the pandemic had put in the front of peoples’ minds: Will it kill us? Getting the answers would be difficult. Viruses were obligate parasites — that is, totally dependent on living cells. Researchers trying to study them struggled with the challenge of keeping them alive outside a host species.
The British effort focused on canine distemper as an animal model for influenza, using dogs and later ferrets as experimental animals. By 1927, they were testing a distemper vaccine in a two-shot sequence, first with the killed virus, then with the live virus. By 1931 it was available commercially — for dogs. “Is it too much to ask,” the Times (London) wondered, peevishly, “that work on similar lines should be undertaken on the cause of influenza? … Has not the time arrived to launch a campaign and to come to grips with the enemy?”
In fact, researchers were already doing just that. In 1933, at Britain’s National Institute of Medical Research, workers filtered throat washings from flu patients, used the filtrate to infect ferrets, and identified the culprit as the influenza A virus. Soon after, a researcher at the Rockefeller Institute in New York used the same technique to identify a second potential culprit, influenza B. At Vanderbilt University, researchers devised a way to grow viruses apart from their normal host species, using fertilized chicken eggs. Max Theiler (1899–1972), a South African–born researcher at the Rockefeller Foundation in New York, soon put this technique to work developing an effective live attenuated vaccine against yellow fever. Other researchers used the new technique to develop and improve the first flu vaccines. Having risen up and become strong on the bones of the tens of millions lost to the 1918 pandemic, the science of viruses would go on to save hundreds of millions from premature death in the decades just ahead.
Richard Conniff is a National Magazine Award-winning science writer who has written for Smithsonian magazine, The Atlantic, National Geographic, and other publications. He is a past Guggenheim Fellow and the author of several books, including “The Species Seekers: Heroes, Fools, and the Mad Pursuit of Life on Earth,” “Swimming with Piranhas at Feeding Time: My Life Doing Dumb Stuff with Animals,” “The Natural History of the Rich: A Field Guide,” and “Ending Epidemics: A History of Escape From Contagion,” from which this article is excerpted.



