The Future of Fertility Technology, From Technosemen to Uterine Transplants
Fertility technology is an area of intense interest, in which scientists continue to push the boundaries of a human body’s capability to generate the matter that will produce a healthy, living child. It is, unsurprisingly, an area of rapid scientific and technological research — so much so that regulatory bodies across the world have difficulty keeping up-to-date with the latest developments in order to regulate their use properly.
The following excerpt from the conclusion of “Fertility Technology” describes some of the methods that scientists and for-profit companies are testing and offering to patients and clients who are willing to try (and to fund, often at great expense) cutting-edge but unproven techniques to raise their chances of having a baby. This excerpt also draws attention to individuals who need extra assistance with conceiving but for financial, health, or ethical reasons do not want to engage with the latest techniques. Some techniques that were available in the 19th century, like artificial insemination, still can work — backed by updated forms of medical technologies. There is no lack of attention to this area of scientific and technological development, from prospective parents, from scientists, from sperm and egg banks, from international transit companies, from potential donors, from ethicists — and indeed from anyone engaged in questions of how humans will appear in the future.
Semen and Technosemen
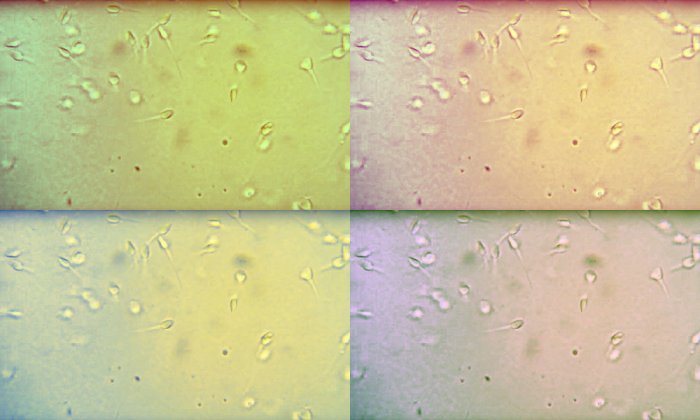
The health of sperm remains an important area of diagnostic concern. Among a host of other issues, low sperm count, low motility, and sperm antibodies (proteins that damage or kill sperm) are all sources of infertility. Sperm health is difficult to treat, but some workarounds for those with at least some healthy sperm do exist. These include testicular sperm extraction and testicular sperm aspiration, using high-powered needles and delicate microsurgical instruments. Physicians can also perform testicular mapping, where they use fine-needle aspiration to try to find “pockets” of sperm production in the testes.
In addition to technologies that can help manifest pregnancy, the gametes, or reproductive cells, themselves can be thought of as technologies. This is true of technosemen, or semen that has undergone laboratory manipulation to be suited especially for intra-cytoplasmic sperm injection (ICSI), where a single healthy sperm is injected directly into each mature egg, and IVF, where an egg is combined with sperm in vitro. Researchers Matthew Schmidt and Lisa Jean Moore have called it “the ‘new and improved’ bodily product that semen banks advertise to clients.” The methods for technosemen manipulation are various. The swim-up method, for example, involves “centrifuging the semen sample, removing the seminal fluid, and placing the remaining sperm pellet in an artificial insemination medium,” and then collecting the most active semen, which “swim” to the top of the solution. Another method is Percoll washing, which involves layering the semen with a cleansing solution and centrifuging it for half an hour.
Washed technosemen is perceived as healthier and more potent than natural, unmanipulated semen.
The ability to manipulate and to choose the best semen affects how clinics view their donors, their donations, and the children who might result from them. For example, in advertising materials for the Danish company Cryos, “semen is solely described in light of the technology involved,” writes researcher Charlotte Kroløkke. “Traces of the matter are reworked into sophisticated technology, beautiful children and indeed — and not surprisingly — happy, healthy, potent donors.” This view that semen is a technoscientific product, not a body product, likewise manifests in China, where the country’s Ministry of Health established specific requirements for technosemen under national law from 2001 to 2003. The Ministry requires a concentration standard of 60 million sperm cells per milliliter, which is four times higher than the World Health Organization’s criteria for normal male fertility, according to anthropologist Ayo Wahlberg, who published a detailed study of sperm-banking in China. A range of “technologies of assurance” quantify spermatic quality not only according to sperm per milliliter, but also “motility grades, percentages of normal morphology, and milligrams of fructose per milliliter.” Then, only the best sperm is used to make the “best quality” children.
The ability to test spermatic health is a means of managing the effects of environmental pollution on the next generation as well. In cities like Wuhan, one study found, semen donated on days with high levels of air pollution showed lower sperm count and concentration than semen donated on days with lower levels of air pollution. Washed technosemen is perceived as healthier and more potent than natural, unmanipulated semen. (Whether it leads to healthier children is much harder to discern.) Sperm banks can then “make claims about the potency of their products, while at the same time making claims as to the ‘naturalness’ of new reproductive technologies,” writes Lisa Jean Moore in her book “Sperm Counts.” “These constructions suggest that new reproductive technologies are not unnatural but rather an improvement upon the inherent unpredictability of natural procreation.” In other words, “the best semen is not natural; it is processed and refined through technology.”
Add-Ons: Time-Lapse Imaging
Like many areas of medicine, reproductive medicine attracts inventors and entrepreneurs. Some of their solutions may provide valid diagnostic information or improve chances of pregnancy but are not yet tested or approved by medical regulatory bodies. Some can be added to standard IVF treatments or are offered as part of comprehensive fertility medicine packages that may not be necessary for all patients. These add-ons can be problematic, as “IVF patients may not be adequately informed about the benefits and risk of IVF add-ons or may not be aware of the paucity of supportive evidence for safety and effectiveness,” according to findings from a recent survey. As navigating the world of add-ons may be confusing even for knowledgeable clients, some countries’ regulatory bodies provide guidance. The UK’s Human Fertilisation and Embryology Authority (HFEA) publishes a traffic-light system, which rates add-ons according to available cost implications, risks, and evidence. A green light indicates that a treatment has shown positive results according to at least one randomized control study, an amber light indicates mixed results, and a red light indicates no positive results. Reviews of add-ons available since 2015 show their overall limited benefit and potential unknown harms to patients.
A survey taken in June and July 2020 showed that up to 24 add-ons were available at clinics across Australia, many of which mirrored those available in the UK. They ranged from mild and complementary (aspirin, acupuncture) to loosely linked (melatonin) to highly technological (assisted hatching). Another review of 10 add-ons, from screening hysteroscopy (examination of the uterus under anesthesia) to androgen supplements, found either that they had no effect on implantation or live birth rates or that there was insufficient data to support such a claim. A third review of five add-ons solely for the endometrium (mucus membrane lining the uterus) showed that their effects ranged from unclear (vasodilators such as sildenafil [Viagra] to thicken the endometrium) to harmful (endometrial scratching, which inflames the endometrium and might make the embryo more likely to implant). These reviews caution that profit may motivate clinics “to provide costly IVF add-ons with no evidence base.”
One of the add-ons that has received the most attention from scholars and fertility medicine specialists is time-lapse imaging, and as such, it is valuable to examine its implications in detail. Time-lapse imaging of embryos from fertilization to three days afterward (for double embryo transfer) to five days afterward (for single embryo transfer) is designed to help embryologists choose the healthiest possible embryo for implantation. Time-lapse imaging technologies, explains Lucy van de Wiel in her exploration of the world of egg freezing, “allow for continuous observation by taking photographs every 5 to 20 minutes while the embryos remain in the incubator. . . . By matching the videos with growth patterns of embryos that developed into healthy fetuses, the time-lapse system suggests which embryos are most likely to grow into a baby.” The time-lapse systems film the developing embryos and quantify the visual information onto grids, and then clinicians must have specialized training in algorithmic analysis to predict each one’s likelihood of turning into a blastocyst, or a fertilized egg. These systems, called EmbryoScope (manufactured by Vitrolife) and Eeva (short for Early Embryo Viability Assessment, manufactured by Merck), depend on past selections to predict future embryo viability. In a May 2019 survey of fertility clinic websites in the United Kingdom, time-lapse imaging costs an average of £478 as a stand-alone treatment and an average of £4,020 as part of a treatment package. The systems themselves cost clinics £75,000–80,000.
Reviews caution that profit may motivate clinics “to provide costly IVF add-ons with no evidence base.”
Time-lapse imaging alters more than just the process of embryo selection. As van de Wiel writes, “by matching the embryos’ cellular growth patterns to previous embryonic populations’ recorded developmental rhythms, time-lapse technology brings embryonic aging to the forefront in embryo selection.” Time-lapse imaging turns embryo selection into a “new, data-driven way of seeing” using “automated pattern recognition and algorithmic predictive analysis.” This process not only changes how laboratory technicians and embryologists see and choose embryos for implantation, but it also changes how a prospective parent or parents see their embryos: “Ranking means that the woman or couple has a quantified sense of the blastocyst’s potential for development,” researcher Catherine Waldby points out.
HFEA gives time-lapse imaging an amber light, as “being undisturbed while they grow may improve the quality of the embryos but there’s certainly not enough evidence to show that time-lapse incubation and imaging is effective at improving your chance of having a baby.” Before getting a green light from HFEA and other national regulatory agencies, time-lapse imaging needs more proof to support Vitrolife’s and Merck’s claims that their products improve embryo selection. In general, inventors and suppliers of new add-ons may be pursuing not only patient satisfaction and profit but also the satisfaction of developing an IVF breakthrough technology to improve implantation and live-birth success rates markedly.
In Vitro Maturation and MDNA Transplantation
Another high-technology method currently being developed involves obtaining functional gametes from either human embryonic stem cells or induced pluripotent stem cells, which are derived from skin or blood cells, and the use of mitochondrial DNA from a donor egg to manifest so-called three-parent embryos. For the latter, “women with healthy mitochondrial histories are asked to donate their eggs to women with family histories of disease, and the recipients’ nuclear genetic material is transferred to the healthy egg,” explains Waldby. “This enables the recipient to conceive a child who is genetically her own, if the terms of genetics are limited to nuclear DNA.” The embryo is then the product of three people’s gametes, containing the nuclear DNA of the intending parents and the mitochondrial DNA of an egg donor. The UK’s Human Fertilisation and Embryology Act (1990) was amended in 2015 to legalize this procedure, called MDNA transplantation; the United Kingdom is the only country that permits it.
The procedure is intended to help women with mitochondrial disorders — often undetectable in preimplantation genetic testing (PGT) — avoid passing those disorders onto potential children, and to ensure that those children are their genetic offspring. Unfortunately for the further acceptance of this procedure, one study found, “most maternally inherited mitochondrial disorders only develop in adulthood, whereas mitochondrial disorders that severely affect babies are caused, in approximately 80% of cases, by nuclear defects that are inherited from both parents.” In other words, replacing mitochondrial DNA alone cannot prevent diseases inherited from both parents, and the procedure helps only in the 20 percent of diseases that are only inherited maternally. The procedure also carries further risks:
[1] the potential side-effects caused by the co-existence of two different types of mitochondria within the embryo’s cytoplasm, including the possible carry-over of pathogenic mtDNA; [2] the possible defects caused by mismatching the nuclear and mitochondrial genomes, such as metabolic dysfunction and epigenetics effects; and [3] the social and psychological consequences of having been conceived using genetic material from three people.
Access to the procedure is heavily restricted, and disorders can often be found in gametes more easily and cost-efficiently using an older diagnosis method, PGT. The ethical considerations of procedures like IVM and MDNA leave many open questions about their use, especially if more problems with them are identified and more countries legalize them.
Uterine Transplants
Another significant technological step is IVF in persons with transplanted uteri. The first modern attempt at a uterine transplant alone took place in Saudi Arabia in 2000. The first IVF procedure in a transplanted uterus from a live donor that resulted in a live birth happened 14 years later in Gothenburg, Sweden. The first live birth via IVF in a uterine transplant in the United States occurred in 2017, and the IVF-transplant procedure has resulted in 70 uterine transfers with 14 live births worldwide as of June 2021. Uterine transplants have been a focus of reproductive medical attention in the last two decades. If the transplant is successful, the donated uterus is removed after a certain period of time and number of successful IVF pregnancies — a number that the patient would determine.
The IVF-transplant procedure has resulted in 70 uterine transfers with 14 live births worldwide as of June 2021.
Uterine transplantation is an intricate procedure, involving immunosuppressant drug regimens, the risk of organ rejection, the possible development of a thrombosis, and other complications. Connecting the blood vessels of the donated uterus to those in the recipient’s body is particularly tricky. But there are many other steps before the transplant and IVF can begin. On the practical side, there is no uterine donation registry, so in the case of live donation, the person without a uterus must ask a prospective donor for theirs (or the prospective donor must offer). Transplantation from a nondirected (anonymous) living donor or a deceased donor is also possible, though familial donors with identical blood types lower the risk of rejection. For some studies, prospective transplant recipients must secure their own donor. Interviews with 10 uterus-seekers in Sweden described how they reached out to their mothers as well as older sisters or aunts, raising the possibility that they could gestate a child using the same uterus in which they themselves were gestated. The emotional intricacy of asking (and possibly receiving) an organ donation in this situation is obvious.
Familial complexities aside, IVF in uterine transplants sparks the possibility of gestating pregnancies outside the human body completely in artificial wombs (ectogenesis). Research on human ectogenesis is still illegal in the United Kingdom, but animal research has been in progress there since the early 1960s. For humans, writes legal scholar Amel Alghrani, “technology that can mimic the functions of the maternal uterus can help save the lives of extremely premature babies born on the cusp of viability. . . . Such technology can also help women who suffer from uterus factor infertility and thus are unable to gestate their own child.” Research is underway in Sweden (by the same team that facilitated the first uterine transplant) to create a viable bioengineered uterus, including artificial amniotic fluid and an artificial endometrium. A bioengineered uterus could also be used for part of a pregnancy; for example, gestation could begin in the human womb, with the fetus transferred later to the artificial one. Successful human ectogenesis, whether wholly or partially gestated in an artificial uterus, could open up a new world of possibilities of reproduction.
Farther in the future is in vitro gametogenesis (IVG), the creation of gametes using pluripotent stem cells (cells that can differentiate into many cell types). If a patient cannot provide gametes for an assisted reproduction treatment, IVG could create gametes from their skin cells. “Artificial gametes,” writes Alghrani in her book on regulating assisted reproductive technologies, “raise ‘one of the most dramatic possibilities that two men (and maybe also two women) could create a baby that is genetically related [to] both of them, in the same way as men and women.’ Artificial gametes widen procreative possibilities for those unable to reproduce via traditional methods of sexual reproduction.” As a result, a couple of any gender could provide all the gametes needed to produce an embryo that is genetically related to both of them.
Historical Technologies 2.0
Of course, child-seekers will continue to use less advanced technologies alongside technologies that require advanced medical assistance and infrastructures. Technologies and methods with historical longevity, such as fertility calendars and home-based insemination, will coexist alongside advances in high-technology methods. Home-based insemination persists especially in countries where access to assisted reproductive technologies is restricted or illegal for some identity groups (usually gay, trans, non-binary, and lesbian individuals). They may find assistance in printed or Internet guides to doing so, which originate in the feminist women’s health movements of the 1970s. Lesbian insemination guidebooks have been in print since 1979, and syringes, cannulas, cervical caps or diaphragms, eye droppers, and jars are available to anyone who purchases them from a medical supply store or online.
People who want fertility assistance, but on their own terms, choose methods that do not violate their own boundaries. They develop “hybrid-technology practices,” as Laura Mamo of the Health Equity Institute calls them, or practices of borrowing from both high- and low-tech methods according to their own health and preferences. Whether it’s through ovulation timing, smartphone apps, or “smart jewelry,” individuals and couples have a range of options for charting their own journeys through the fertility landscape — as long as they have the time, patience, finances, and good health to do so.
A history of fertility technologies can only hint at the vastly complex ways that the desire for children affects the lives of individuals, couples, communities, and nations. The technologies that make pregnancy possible for some people are a source of disappointment for others. They are means of giving certain embryos a chance to develop as persons in the world, but also a means of keeping other embryos and potential persons out of the world. Fertility technologies are much more than a way to address reproductive health problems or “simply a medical procedure to cure a medically described condition,” as Sandra P. González-Santos reminds us. They are “a tool through which people create people.” How they will develop next — and what kinds of human life will emerge as a result of using them — remains to be seen.
Donna J. Drucker is Assistant Director of Scholarship and Research Development at the Columbia University School of Nursing. She is the author of “The Classification of Sex: Alfred Kinsey and the Organization of Knowledge,” “The Machines of Sex Research: Technology and the Politics of Identity, 1945–1985,” “Contraception: A Concise History,” and “Fertility Technology,” from which this article is adapted.



