The Art of Living and Dying With Cancer: In Conversation With Dr. Robert Schneider

As part of the research for “Beatriz da Costa: (un)disciplinary tactics,” curator Daniela Lieja Quintanar and curatorial assistant Ana Briz traveled to New York in August 2022 to interview Dr. Robert Schneider, a professor of radiation oncology and the co-director of the Breast Cancer Program at the Grossman School of Medicine at NYU. Seated in Dr. Schneider’s office at the NYU Langone Health center, they discussed his experience treating the artist Beatriz da Costa for her rapidly metastasizing breast cancer from 2011 to 2012.
During da Costa’s treatment with Dr. Schneider and his team, an unexpected collaboration developed between the artist and the scientist. Their work together extended not only to her health and longevity but also influenced her artistic process. The curatorial team was interested to learn more about Dr. Schneider’s role in da Costa’s series, “The Cost of Life” (2011–13), which explores the artist’s battle with cancer and proposes alternative forms of healing. In “Dying for the Other” (2011), the first video in the series, which was partially filmed in one of Dr. Schneider’s laboratory facilities, da Costa intertwines her own life with that of lab mice used for scientific research, illuminating the nuances of illness, therapeutics, and interconnectedness between humans and animals. On a tour of Dr. Schneider’s lab, the curators met with scientists studying the progression of breast cancer on a molecular level, who use those results to conduct new clinical therapeutics for the disease.
The following conversation, edited for length and clarity, highlights the personalized approach that Dr. Schneider and his colleagues provide to patients like da Costa within a medical landscape often characterized by standardization. The convergence of art and science described, and the necessity for innovation and creativity within both disciplines, is essential to understanding the human experience and finding ways to heal within it.
—Nadia Estrada
DANIELA LIEJA QUINTANAR: We’re interested in learning how you met Beatriz.
ANA BRIZ: What were you working on at the time?
ROBERT SCHNEIDER: I was an Associate Director of the NYU Cancer Institute and Director of Translational Cancer Research, a merger between medicine and science, the goal of which is to find new treatments and therapeutics in cancer. I was also co-directing the Breast Cancer Program, along with Dr. Franco Muggia, and Dr. Silvia Formenti who was then the Chair of Radiation Oncology.
I’m also a professor in radiation oncology. We converged the latest scientific discoveries with medicine for patients where we had nothing left to offer them. It was not acceptable for us to give up. Franco would say to me, “Bob, pull some science out of your hat, let’s figure out what we can do here.” That was an extraordinary time.
DLQ: What year was that?

RS: It was from 2008 to 2017. It was at that time that I received a call from Beatriz. She explained the issue, that everybody had given up on her. She had Hodgkin’s lymphoma as a young teenager. Lymphoma is a liquid tumor often found in the lymphatic system around the lungs and the treatment at that time, which is no longer used, was radiation, including to the chest. It was effective, except that many of these young women later developed breast cancer — likely due to the radiation to the chest — and because of the doses of radiation they typically were very aggressive cancers.
When we met Beatriz, her breast cancer had already metastasized to her brain. Not only do we have so few therapeutics that work on metastatic diseases to begin with, but once metastases are in the brain, we have even fewer and none can be said to be curative. Certainly, most immunotherapies don’t get into the brain very well unless we do intrathecal,1 and that leaves us with few options. A major therapy for brain metastasis is stereotactic radiosurgery,2 which is basically gamma radiation precisely aimed to destroy metastases, but it can only be done so many times.
It was rare to find someone who really understood that art and science are very similar. You’re working for years and you don’t know how it will end. Art is the same way.
Silvia worked out a way to conduct stereotactic radiotherapy on Beatriz’s numerous metastases, which was somewhat effective. Franco and I worked out a drug treatment strategy to complement the radiation therapy. Beatriz went into this knowing that this was palliative — she said, “I’ll be your guinea pig.” We got to know her really well over about two years that we kept her alive. She loved life. She wanted to live. In the course of meeting with her, we had many discussions about art and science. It was rare to find someone who really understood that art and science are very similar. People think about science as a process of linearly plodding along — and yes, a lot of science is done that way, but not by everyone, and not if we struggle for innovation. In science, I think to really be innovative requires the same kind of imagination that you use in art. It’s not at all surprising that so many scientists love art or are artists themselves, right? Because it’s part of the same process of creativity: making connections, connecting dots that nobody else sees. It takes a lot of fortitude because there’s a lot of anxiety when you’re conducting science innovatively. You’re working for years and you don’t know how it will end. Art is the same way.
DLQ: Totally. Beatriz’s artistic practice flowed back and forth between art and science. She collaborated with humans and nonhumans similarly, just as your team worked with her and the mice.
RS: Beatriz really understood how the two species were so highly integrated, and she loved science. She never restricted herself to any art form. She understood the science she was interested in, which was rather remarkable. How did you come to find me?
DLQ: Robert Nideffer, her former partner, mentioned you because we wanted to speak with a scientist collaborator. He pointed out how you allowed her to film in your laboratories.
AB: I believe she created a video triptych here about cancer called “Dying for the Other.”
RS: Yes, we treated her at NYU, and she spent time in my lab sort of poking around and talking to people. I forgot all about this.
AB: She did some of that film and then made a whole series called “The Cost of Life.” She made a couple of pieces around this time: she had “The Life Garden” — which contained medicinal herbs and vegetables — then held cooking workshops thinking about food and wellness as part of “The Delicious Apothecary.” Finally, she created “The Anti-Cancer Survival Kit,” made up of different materials, games, and literature that her friends and collaborators completed after her death. Something that has been continuously worked on since then is a resource database on holistic illness treatments. Surely you two might have had conversations about that.
RS: I think a key part of all this is how much she wanted to live. Shortly before she died, she actually said, “Bob, I just want a few more days, a few more hours.”
DLQ: Tell us more about when you met her, what were your first impressions?
RS: I didn’t know who Beatriz was.
AB: She reached out to you?
RS: Yes, she was a shock to me. She was unusual and very outgoing. At first, I wasn’t sure whether I wanted to get involved because quite honestly, the last thing I wanted was to be part of her project. But there was something about her that after thirty minutes really captivated me, which was, again, [her] love of life and a real understanding of the process of creation.
DLQ: How did the conversation start about doing the video?
RS: At first I was a little incredulous because I’m thinking, you don’t paint, you do videos — but then [she did] other things, all kinds of things to express [herself]. It took me a while to wrap my mind around it because, while I love art, I’m a little more classical. Then I began to understand why she used so many different types of media. Because that was the best way to express different fusions between the process of creation and science and art, the best way for her to see the world of science and its beauty.
AB: That goes back to imagination. The medium, of course, helps to communicate the message, but at the end of the day it is art through imagination, through that creation.
RS: At some point I realized that while she was trying to capture how art and science work together, the media that she used was actually doing that. The questions she asked were very probing at times. She really made me think.
AB: That was her art, making people think. Was she undergoing treatment at first and then wanted to film?
RS: When we first spoke, she wanted for us to develop a treatment to keep her alive longer and also to do her documentary. She asked if she could film in my lab, and after receiving permission I said of course. I don’t remember much about what she actually filmed, but I know she was here with her cameras and Robert [Nideffer].

DLQ: One of the most impactful scenes for me is a closeup of mice being injected and handled.
RS: That’s right! I had to get approval for her to do that filming. We were working on a drug with a major pharmaceutical company at the time that was sponsoring some of that work for treating cancer in the brain — both primary cancers like glioblastoma3, as well as metastases to the brain. What was extraordinary was her hope that what we were doing would be able to be used on her. She watched how we actually implanted the tumor cells in the brain of a mouse — very precise surgery — then combined radiotherapy and drug treatment.
AB: There’s that juxtaposition in the video of her own life and the life of the mice?
RS: That’s right.
AB: The tumors, the drugs, and the treatments. She also has other portions where Robert [Nideffer] is helping her with her speech.
RS: She was losing speech qualities after radiotherapy, which is not unusual but it was frustrating for her. What had to be really hard was that the mouse was her and she knew what the fate of the mouse was as well. At some point she also said, “Bob, I’m your mouse.” That had to be really difficult.
At some point she also said, “Bob, I’m your mouse.” That had to be really difficult.
DLQ: That connects with the title of the series, “The Cost of Life,” and the video, “Dying for the Other.” It’s deep and sad.
RS: Her great hope was that what we learned from her would be used for others. She understood that she would die, she just wanted a few more years. I think we gave her another one or two.
AB: Around 2010, she was at the University of California, Santa Cruz, working on her PhD, but because of the cancer she moved to New York and spent 2011 and 2012 here [in New York].
DLQ: It’s amazing that she had access to your lab. Usually there’s a barrier to the science happening inside of a university, but she always wanted to bring the lab to the public.
RS: The institution was supportive about it.
DLQ: You mentioned bringing science into medicine. What do you mean?
RS: A problem in medicine is that it’s twenty years or more behind the science and it takes a long time for the practice of medicine to incorporate new discoveries. What we understand in the lab in terms of drivers of disease and how to intervene with those diseases — the therapeutics we develop — can take many years to make their way into medicine between the essential need for FDA approval, further clinical development, and ultimately creating a foothold in medical practice.
The other problem is that our understanding of disease has become much more sophisticated, which means it’s so complex that it’s impossible for any physician to keep up with it all. There are a relentless number of patients needing specialized care and you can’t typically do anything experimental without approval. A physician is going to rely on the approaches, the therapies, and the drugs that are familiar. By bringing science much closer to medicine, we can inform better decisions and have access to more treatment options.
When patients with cancer fail one therapy, there are subsequent lines of treatment. Typically, we get to the experimental therapies when the first or second options fail, once the tumors are resistant to everything. Instead, the science could have an enormous impact if we could move up the experimental therapies to be second in line. It’s not a physician’s fault when they don’t have access to these therapies and it’s so complicated just taking care of patients. But when you have science interacting with treatment on a weekly basis — which is what Sylvia, Franco, and I would get to do — decisions for patients can be based on the experimental therapies that we and others develop.
AB: Yours seems like a much more personal kind of attention.
RS: It’s very much personalized medicine. It’s enormously time consuming, but you have the satisfaction of having a huge impact on the lives of patients and their families.
DLQ: How common is it for someone to have access to experimental treatment like Beatriz did?
RS: Typically, we would consider the patients that were not responding to treatment, who we were really worried about losing. Sometimes patients reached out to us like Beatriz did. I believe she found us because Silvia and I had published some important papers with our colleagues on new experimental approaches that worked well in advanced breast cancer.
AB: I’m wondering about the relationship between treatment and preventative science?
RS: While preventive science and medicine is important, for most people there is little we can do to prevent their cancer occurrence. The problem with focusing so much attention on prevention is that people often blame themselves for their disease. “What did I do wrong? I ate well. I exercise. I must have done something wrong.” You didn’t do anything wrong. Let’s face it, you should eat well. You should reduce your red meat consumption. You should exercise. But you may still develop breast cancer because of your genetics, because of exposures you cannot control. What we really need are better therapies for people who present with late-stage disease, which is where we continue to fail.
AB: She was concerned with questions of how to treat and prevent, while also addressing environmental and societal factors.
RS: Environmental factors, sadly, we have very little control over. You can do everything right and then you find out that the juices you drink are packaged in plastic treated with BPA. Or that your exposure when you were two years old is what preordained you to actually develop cancer later. Or Beatriz’s case: treated with all the proper intent to cure her Hodgkin’s lymphoma only to discover twenty years later that it gave these women breast cancer.
Most researchers view life as precious, whereas I think the general public thinks of research scientists as being hardened and disrespectful.
DLQ: There are controversies in science about testing treatments on animals versus humans.
RS: Testing on mice is essential for what we do because mice are so well-defined genetically. We can easily track changes in them. It’s easier to cure cancer in a mouse and not in a human because we’re more complex. But if you’re trying to save life, you better respect life and that includes the life of a mouse. So if you’re going to take a life, or many lives of mice, you better make sure that your experiments are designed in a way that you really learn something useful.
AB: I think that was your perspective, that there’s a connection between different species and us as humans, whether it’s treatment on them or us.
RS: Absolutely. We work with mice in this lab every day, but there’s nobody in my group that doesn’t understand the sanctity of life. We always learn something.
DLQ: Beatriz had a piece where she collaborated with pigeons [“PigeonBlog”(2006–08)]. I think she was keen on seeing animals not just as the objects of a study but as collaborators, and how the whole world needs to work in such a sense. Interspecies collaboration instead of the superiority of humans.
RS: Yes, I think she understood that. Most researchers view life as precious, whereas I think the general public thinks of research scientists, especially those in life sciences and biomedicine, as being hardened and disrespectful. It’s just the opposite.
DLQ: The experimental treatments Beatriz received did give her more time. What did you discover while doing these treatments?
RS: In the case of Beatriz, we had very little to work with because she had had so many other treatments, and the treatments that we were able to give her were somewhat more palliative. I remember stereotactic radiotherapy and then we gave her whole brain radiotherapy. We knew we weren’t going to cure her — she knew she wasn’t going to be cured. Frankly, the negotiation with her was that she wanted us to help get her a few more years to finish her art and put things in order. An extra year can mean so much to anybody. You can embrace it and understand that you’ve been given a gift of life. As I said, her words were, “Bob, I just want to live a little longer.”
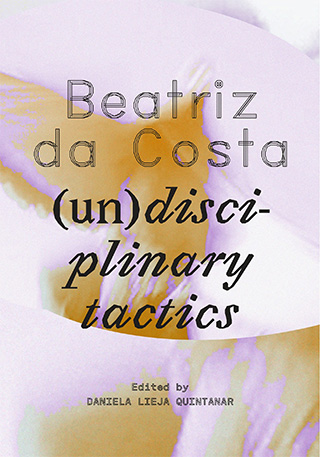
Daniela Lieja Quintanar is Chief Curator and Deputy Director of Programs at REDCAT, former Chief Curator of LACE, and editor of the volume “Beatriz da Costa: (un)disciplinary tactics.”
Ana Briz is Assistant Director and Curator of Exhibitions at the AD&A Museum and Associate Editor of the volume “Beatriz da Costa: (un)disciplinary tactics.”
“Beatriz da Costa: (un)disciplinary tactics,” the volume from which this article is excerpted, accompanied a solo exhibition presented by Los Angeles Contemporary Exhibitions (LACE) from Sept 7, 2024 to Jan 5, 2025, as part of the Getty’s PST ART: Art & Science Collide initiative.
- “Intrathecal” refers to the administration of chemotherapy drugs directly to the cerebrospinal fluid that surrounds the brain and spinal cord, targeting the central nervous system in ways not accessible via radiation or intravenously. “Intrathecal Therapy for Acute Myeloid Leukemia,” Patient Care NYU Langone Health, accessed March 25, 2024
- “Stereotactic radiosurgery” refers to a highly focused radiation treatment that targets a tumor with an intense and concentrated dose of radiation, while limiting the dose to the surrounding organs. “Stereotactic Ablative Radiotherapy (SABR/ SBRT),” Stanford Health Care, accessed March 25, 2024
- Glioblastoma is a type of aggressive cancer that starts with cell growth in the brain or spinal cord. “Types of Glioma & Astrocytoma,” Patient Care at NYU Langone Health, accessed March 25, 2024.



